For countless couples struggling with infertility, in vitro fertilization (IVF) shines as a beacon of hope in the field of assisted reproductive technologies. The word “blastocyst” is of utmost importance in this complex procedure. We will delve deeply into the world of blastocysts in IVF in this comprehensive guide, understanding their significance, formation, definition, and role in successful pregnancies. So buckle up as we set out on this fascinating journey!
Table of Contents
What is blastocyst in IVF?
A blastocyst is an advanced stage of embryo development in the context of in vitro fertilization (IVF), which takes place 5-7 days after fertilization. The fertilized egg, also known as a zygote, goes through several rounds of cell division and differentiation at this stage, resulting in a structure with between 70 and 100 cells.
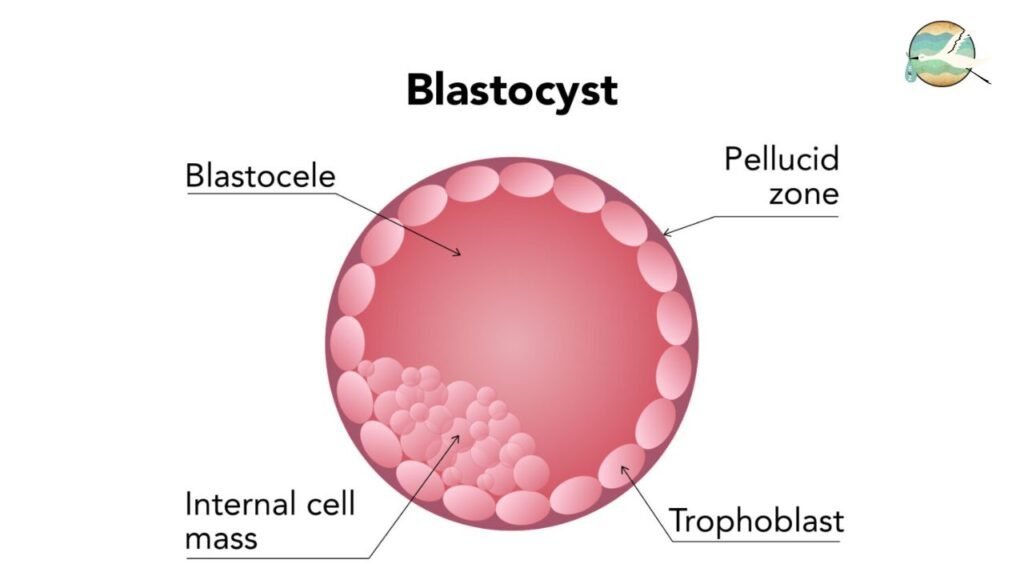
The blastocyst is characterized by two main components:
Trophoblast: The placenta, which supplies oxygen and nutrients to the growing embryo, will eventually emerge from this outer layer of cells.
Inner cell mass (ICM): This collection of cells, which can be found inside the trophoblast, will eventually develop into the fetus.
Because it indicates the point at which the embryo is prepared to implant into the lining of the uterus, the blastocyst is a crucial developmental stage in IVF. Embryos are typically cultured in a lab setting for a few days following fertilization as part of a standard IVF procedure before being placed in the uterus. Fertility specialists can choose the healthiest, most viable embryos for transfer in order to increase the likelihood of successful implantation and pregnancy by letting embryos develop to the blastocyst stage before transfer.
By allowing embryologists to see which embryos are displaying the most typical growth and development, choosing to transfer blastocyst-stage embryos also offers the benefit of better embryo selection and raises the possibility of a successful pregnancy.
Step-by-Step Guide to Blastocyst Transfer
- Ovarian Stimulation: Ovarian stimulation, which promotes the growth of numerous follicles, is the first step in the IVF process.
- Egg Retrieval: The ovaries are harvested using a minimally invasive procedure to retrieve mature eggs.
- Fertilization: In a lab setting, the retrieved eggs are fertilized with sperm.
- Embryo Culture: To enable the development of fertilized eggs into blastocysts, they are cultured in a regulated environment.
- Blastocyst Grading: The quality and developmental stage of embryos are used to assign grades.
- Blastocyst Transfer: The transfer of high-quality blastocysts into the uterus is chosen.
- Pregnancy Test: About two weeks after the transfer, a pregnancy test is done to see if implantation was successful.

How many cells in a blastocyst
Normally, a blastocyst contains between 70 and 100 cells. The trophoblast, which will give rise to the placenta, and the inner cell mass (ICM), which will develop into the fetus, are the two main cell types organized at this stage of development. The ICM is a collection of cells located inside the blastocyst, whereas the trophoblast is made up of many cells that surround a cavity filled with fluid. Although the precise number of cells can differ between individual blastocysts, the above range is a rough estimate.
How many 8 cell embryos make it to blastocyst?

Depending on variables like the quality of the embryos and the particular lab conditions, the development of embryos from the 8-cell stage to the blastocyst stage can vary significantly. Generally speaking, not every 8-cell embryo will successfully form a blastocyst.
According to estimates, under ideal circumstances, 30–50% of 8-cell embryos might develop to the blastocyst stage. According to unique factors, such as the woman’s age, the quality of the embryos, and the team’s expertise in embryology, this percentage may, however, differ significantly from case to case. At different stages of development, some embryos may stop developing, while others may grow into blastocysts with a high chance of implanting.
The development of embryos is carefully tracked by embryologists, who then choose the most viable ones for freezing or transfer. Increased chances of successful implantation and pregnancy are the main objectives.
When to do Pregnancy test after blastocyst transfer
It is typically advised to hold off on a pregnancy test for 10 to 14 days after a blastocyst transfer during an IVF procedure. This waiting period provides enough time for the embryo to successfully attach to the uterine lining and for the body to begin producing detectable levels of the hormone hCG (human chorionic gonadotropin), an early indicator of pregnancy.
A false negative result can be obtained by administering the test too soon before the hCG levels have had a chance to rise. By holding off until the advised window of time, you can improve the pregnancy test’s accuracy and lessen the chance that incorrect results will leave you perplexed or disappointed.
However, it’s crucial to adhere to the precise instructions and advice given by your doctor or fertility clinic, as they may have their own preferences or protocols regarding when to perform a pregnancy test following a blastocyst transfer.
Which layer of blastocyst gets attached to the endometrium?
When a blastocyst is implanted, its outer layer, or trophoblast, which is also known as the trophoblast, fuses to the endometrium (the uterus lining). The placenta, a vital organ that supplies nutrients, oxygen, and support to the growing embryo and fetus throughout pregnancy, is formed by the trophoblast. The interaction between the endometrium’s cells and the trophoblast cells during implantation enables the embryo to connect to the mother’s blood supply and start growing and developing.
Conclusion: Blastocyst in IVF
The blastocyst stage is a crucial one in embryo development when it comes to IVF. Due to the longer cultivation period that enables better embryo selection, choosing blastocyst transfer can result in higher pregnancy rates. Understanding the significance of blastocysts and their function in the IVF process can empower you to make wise decisions and raise your chances of a successful pregnancy as you start your IVF journey. Remember, the best way to choose the best course for your particular situation is to discuss your options with a qualified fertility specialist.
Related Post:
- What is Sperm Cramps?
- Does Female Masturbation Increase Fertility?
- Are Painful Periods a Sign of Good Fertility?
- What Happens If a Man Releases Sperm Daily?
FAQs about Blastocyst in IVF
Q1: Why is blastocyst development important in IVF?
Development of the blastocyst indicates a healthy, mature embryo. To increase the probability of a successful pregnancy, it makes sure that only the most viable embryos are chosen for transfer.
Q2: How is blastocyst development achieved?
Embryos are cultured in a controlled environment for a few days following fertilization so they can transform into blastocysts. This prolonged cultivation period imitates the fallopian tubes’ organic process.
Q3: Is transferring blastocysts better than earlier embryos?
The success rates for transferring blastocysts have indeed been higher. These embryos have already gone through significant developmental phases, demonstrating their potential for successful implantation.
Q4: Are there any risks associated with blastocyst transfer?
Although blastocyst transfers typically have a high success rate, there is a chance that more than one transfer could result in multiple pregnancies. Patients and their healthcare providers should talk about how many embryos will be transferred.






[…] What is blastocyst in IVF? […]