Trying to figure out when your body is most likely to conceive can feel confusing—especially when social media throws around terms like “egg-white mucus,” “LH surge,” and “mittelschmerz.” This guide explains the real, reliable signs of high fertility in a woman, what they look like in everyday life, and how to use them to time intercourse with confidence. You’ll find plain, friendly language, Indian English, and practical steps you can start using right away.
First, what “high fertility” actually means
When people say “high fertility days,” they’re talking about the fertile window—the short stretch each cycle when sex is most likely to lead to pregnancy. Pregnancy is possible during a six-day window: the day of ovulation (when your ovary releases an egg) and the five days before it. That’s because sperm can live in the female reproductive tract for up to five days, while the egg lives for about 24 hours after ovulation. The chance of conception rises as you get closer to ovulation and tends to be highest on the day before and the day of ovulation.
Two practical takeaways:
- Focus on the days leading up to ovulation, not only the day itself.
- Your fertile window shifts with your cycle length. Ovulation commonly happens 10–16 days before your next period, not magically on day 14 for everyone.
The most reliable signs of high fertility (and how to track them)
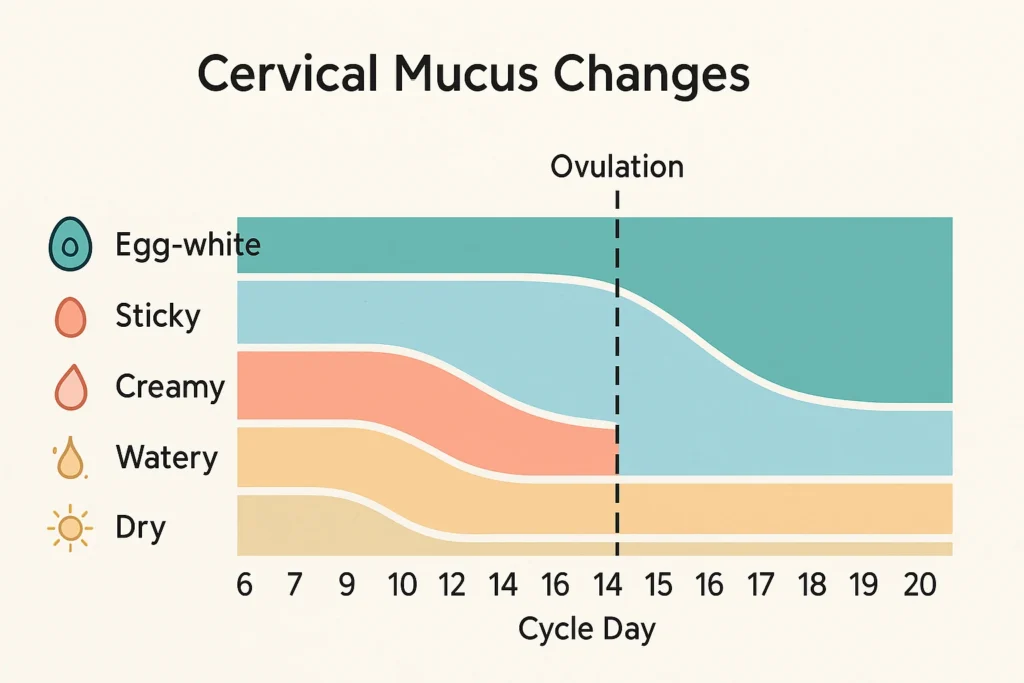
1) Clear, slippery “egg-white” cervical mucus (EWCM)
- What you’ll notice: Vaginal discharge increases and becomes clear, slippery, and stretchy—often compared to raw egg white. You might see it in your underwear or when you wipe.
- Why it matters: Rising oestrogen before ovulation transforms the cervix and its secretions to help sperm swim, survive, and reach the egg. This type of mucus is a strong, natural sign that your fertile window is open.
- How to track it well: Check mucus daily using clean fingers and good light. Pay attention to texture (slippery/stretchy) and sensation (wet/slippery at the vulva), not colour alone.
- What to do: If you notice fertile-type mucus today or yesterday, consider yourself in the fertile window. Having sex every day or on alternate days while this mucus is present is a practical approach.
Tip: Many people don’t see much cervical mucus on the underwear but do notice it when they wipe or check internally. If you rarely see “egg-white” mucus externally, you can still use other signs like LH tests.
2) A positive LH surge on an ovulation test (OPK)
- What you’ll notice: A home urine test shows a positive line or a digital “peak.” This detects a surge in luteinising hormone (LH) that usually occurs about 24–36 hours before ovulation.
- Why it matters: LH is the trigger that tells your ovary to release an egg. A positive OPK means ovulation is likely soon.
- How to track it well: If your cycles are around 28 days, start testing by day 10–11. If your cycles are longer, start earlier; if shorter, start later. Test at roughly the same time each day, and avoid very dilute urine.
- What to do: Time intercourse on the day of your positive test and the following day. Pair OPKs with mucus tracking for the clearest picture.
Note for PCOS: Some people with PCOS have consistently higher LH levels, causing confusing or false positives. Combine OPKs with mucus observations and consider cycle-tracking with a clinician if your cycles are very irregular.
3) Mid-cycle one-sided pelvic twinge (“mittelschmerz”)
- What you’ll notice: A brief, one-sided ache or twinge low in the abdomen, typically around your mid-cycle.
- Why it happens: The growing follicle stretches, and when the egg is released, a small amount of fluid or blood can irritate nearby tissues.
- How to use it: This is a secondary sign—use it to support what your mucus and OPKs are telling you, rather than as your only tracker.
- When to seek help: If pain is severe, persistent, or accompanied by fever, vomiting, or heavy bleeding, please seek medical care to rule out other causes.
4) Basal body temperature (BBT) rise — confirms ovulation after it happens
- What you’ll notice: A small, sustained increase in your waking temperature (about 0.3 °C; 0.5–1 °F) after ovulation, caused by progesterone.
- Why it matters: BBT doesn’t predict ovulation; it confirms that ovulation has already occurred. It’s most useful for understanding your own pattern across cycles.
- How to track it well: Take your temperature first thing on waking, before you sit up or drink water, ideally at the same time every day. Look for a sustained rise across at least two to three days.
Signs that are possible but less reliable on their own
- Cervix position and feel: Near ovulation, the cervix can feel softer, higher, and slightly open. This can be helpful, but is harder to assess consistently and varies from person to person.
- Breast tenderness, bloating, mood changes, shifts in libido or senses: Some people notice patterns, but these symptoms are non-specific. Use them only as minor clues.
- Saliva “ferning” gadgets: These can sometimes show patterns linked to oestrogen, but results are variable. Treat them as bonus information, not a stand-alone method.
One-glance guide: signs of high fertility and what to do
| Sign you can track | What it looks/feels like | What it usually means | How reliable for timing?* | What to do |
|---|---|---|---|---|
| Cervical mucus becomes clear, slippery, stretchy | “Egg-white” texture; more abundant | Oestrogen is high; fertile window is open | High (predictive when present) | Have sex daily or on alternate days while present |
| Positive LH test (OPK) | Test line or digital “peak” | LH surge → ovulation in ~24–36 h | High (predictive) | Have sex the day of the surge and the next day |
| Ovulation pain (mittelschmerz) | One-sided pelvic ache/twinge | Ovulation may be occurring | Moderate (supporting sign) | Use alongside mucus/LH; seek care if severe |
| BBT rise | ~0.3 °C sustained increase next mornings | Ovulation has already happened | Good for confirmation | Use to learn your pattern; not for same-cycle timing |
*“Reliability” here means usefulness for identifying the fertile window when used correctly and consistently.
How to put it all together (a simple, step-by-step plan)
Let’s assume Day 1 = the first day of bleeding. Adjust the timeline to your own cycle length.
- Start watching mucus right after your period. As soon as it shifts from dry/sticky to wet/slippery/stretchy, assume you’re in your fertile window.
- Begin LH tests several days before you expect to ovulate. With 28-day cycles, start around day 10–11. With 32-day cycles, start earlier (e.g., day 12–13) since ovulation may be later. With 24-day cycles, start sooner (e.g., day 8–9).
- Time intercourse for the two days before ovulation and the day of ovulation. In practice, that often means having sex on the days of peak mucus and the day of/after your LH surge.
- Chart BBT to confirm ovulation happened. You’ll see a small rise in the mornings after ovulation. Over two to three cycles, you’ll learn your personal rhythm.
- Repeat across a few cycles. Most people become more accurate and less stressed with practice.
Context matters: cycle length, age, and health
- Cycle regularity: Cycles between 21 and 35 days are usually ovulatory. If your cycles are very irregular (e.g., skipping months, unpredictable lengths), tracking can be harder, and you may need a personalised evaluation.
- Age: Fertility naturally declines with age due to changes in egg number and quality. If you’re under 35 and not pregnant after 12 months of trying (with well-timed intercourse), consider a fertility evaluation. If you’re 35 or older, seek evaluation after 6 months; at 40 or above, consider early counselling even when you begin trying.
- Health conditions: PCOS, thyroid disorders, high prolactin, endometriosis, untreated STIs, or significant under- or over-weight can affect ovulation and mucus patterns. If any of these apply to you—or you have severe period pain, very heavy bleeding, or cycles shorter than 21 days or longer than 35–40 days—speak with a clinician.
- Post-pill cycles: After stopping hormonal contraception, it may take a few cycles for ovulation signs to become clear. Keep tracking; patterns usually return.
- Breastfeeding and postpartum: If you’re breastfeeding, cycles may be irregular or absent. Ovulation can still occur before your first period returns, so signs like mucus changes are worth watching.
Myths to leave behind
- “BBT tells me when to have sex today.” Not quite. BBT confirms ovulation after the fact. Use it to refine timing in future cycles, not as your only same-day signal.
- “Everyone ovulates on day 14.” False. Ovulation can vary widely. What matters is the interval before your next period (often 10–16 days), not a fixed day number.
- “No egg-white mucus means I can’t conceive.” Not true. Some people don’t see much externally; internal checks or OPKs can still help. Hydration and general health also influence mucus volume.
- “Saliva ferning is enough.” Treat gadgets as add-ons. Your best foundation is mucus + LH, with BBT for confirmation.
Fertility-friendly habits that support ovulation signs
- Have sex across the window: Every day or alternate days when you see fertile-type mucus and/or get a positive LH test.
- Sleep and stress: Consistent sleep, light to moderate movement, and stress-management techniques (breathing exercises, yoga, short walks) help hormone rhythms and make charting easier.
- Nutrition basics: Aim for a varied diet rich in whole grains, legumes, fruits, vegetables, nuts, seeds, and good-quality proteins. Include iron and B-vitamin sources if you have heavy periods. Use supplements only as advised by a clinician.
- Lubricants: Many common lubricants are not sperm-friendly. If you need one, look for products marked as fertility-friendly.
- Medications & herbs: Avoid self-prescribing hormones or herbal “fertility boosters.” Any medication or supplement should follow the clinician’s guidance and official labelling.
When discharge changes are not a sign of fertility
Fertile cervical mucus is typically clear, slippery, and not foul-smelling. Seek medical care if you notice:
- Green or yellow discharge
- Thick, curd-like discharge with itching/burning
- Strong fishy odour
- Pelvic pain, fever, bleeding after sex, or bleeding between periods
These can point to infections (like bacterial vaginosis, thrush, or STIs) or other conditions that need testing and treatment.
Safety reminders (educational, not medical advice)
- Severe lower abdominal pain, fainting, fever, very heavy bleeding, or foul-smelling discharge are red flags—please seek urgent care.
- If you’re under 35 and have tried for 12 months without success, or 35 and older and have tried for 6 months, arrange a fertility evaluation for both partners. Male factors contribute more often than many people realise.
- Routine blood tests like AMH are not accurate “fertility scorecards” for predicting your chances of natural pregnancy outside of a clinical context. Discuss any test results with a qualified clinician.
Putting it into practice: a calm, realistic plan
- Learn your baseline by tracking mucus daily and using OPKs for at least two to three cycles.
- Time sex for the days with slippery/egg-white mucus and on the day of/after your LH surge.
- Use BBT to confirm ovulation and to understand how many days you typically have between ovulation and your period (your luteal phase).
- If timing is clear but conception isn’t happening within the usual time frames, don’t wait too long to speak with a specialist—early guidance can save time and stress.
Bottom line
The most dependable signs of high fertility in a woman are (1) fertile-type cervical mucus, (2) a positive LH test, and (3) sometimes mid-cycle ovulation pain, with BBT confirming that ovulation has already taken place. Use mucus + LH together to spot your fertile days, time sex on those days, and track for a few cycles to learn your unique pattern. If cycles are irregular, you’re over 35, or you’ve been trying without success, a timely check-in with a fertility specialist can make all the difference.