Early-cycle spotting can be confusing—especially if you’re trying to conceive or waiting for your period. Is that faint pink smear an early pregnancy sign, or just your period arriving? This guide explains the real, clinically grounded differences between implantation bleeding and a normal menstrual period, including timing, flow, colour, cramps, testing strategy, and when to seek medical care.
Educational note: This article shares general health information and is not a substitute for personalised medical advice. If you have severe pain, heavy bleeding, feel faint, or are worried about an ectopic pregnancy, seek urgent care.
What is implantation bleeding?
Implantation bleeding is light vaginal spotting that can occur when a fertilised egg attaches to the uterine lining (endometrium). It typically happens about 10–14 days after conception, which is around the time your period would be due if you conceived that cycle. Not everyone experiences it—many healthy pregnancies have no implantation spotting at all.
What it usually looks like
- Amount: “Spotting” rather than a flow—just a few drops, smears, or light staining on underwear or tissue.
- Colour: Often pink or brown. It may look diluted or rusty because the blood is minimal and older by the time it exits.
- Duration: Brief—hours to 1–2 days.
- Cramps: Mild or none. Some people notice a dull ache or twinges.
What is a normal period?
A menstrual period is the shedding of the uterine lining if pregnancy does not occur. A typical period:
- Arrives on schedule for your cycle (most adult cycles are 21–35 days long).
- Lasts 2–7 days.
- Flow pattern: Often light at the start, heavier for 1–3 days, then tapers.
- Colour: Bright to dark red is common; small clots can appear.
- Cramps: Mild to moderate cramps are common in the early days.
If you are soaking pads/tampons/menstrual cups every 1–2 hours, bleeding longer than 7–8 days, or passing large clots, that’s heavy bleeding and worth a gynaecology check.
At-a-glance comparison: Implantation vs Period
| Timing | ~10–14 days after conception; often near the expected period | Cycle day 1, typically 21–35 days after the last period |
| Flow/amount | Very light “spotting”; may be only when wiping | Light → moderate/heavy → light over 2–7 days |
| Colour | Pink or brown; sometimes very faint | Bright to dark red is typical |
| Duration | A few hours to 1–2 days | Usually 2–7 days |
| Clots/tissue | No clots (amount too small to clot) | Small clots can be normal; frequent/large clots suggest heavy bleeding |
| Cramps | Mild or none | Mild to moderate cramps common |
| Other signs | May coincide with early pregnancy symptoms (breast tenderness, fatigue, nausea)—but these also mimic PMS | PMS symptoms (bloating, mood changes, breast tenderness) |
| Pregnancy test | Can still be negative if tested too early; best after a missed period | If it’s a true period, home tests remain negative |
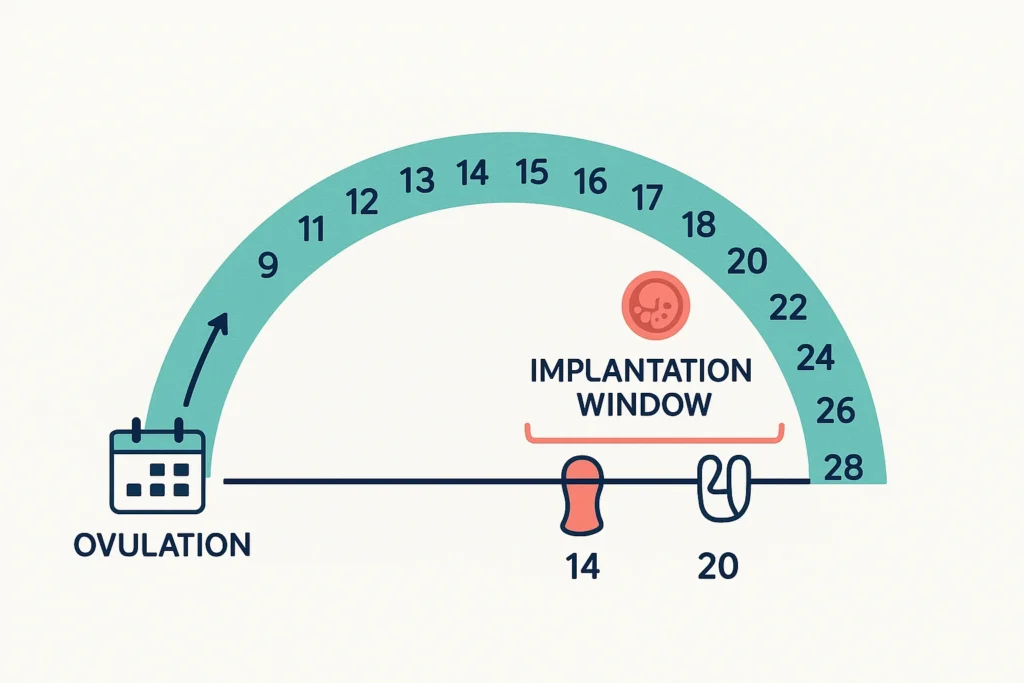
A realistic timeline (example: 28-day cycle)
- Day 14 (approx.): Ovulation.
- Days 20–28 (6–14 days after ovulation): If conception occurred, implantation may happen now. Brief pink/brown spotting could appear shortly before or around your expected period.
- Day 28: Expected period day.
- If you see only a few spots and then nothing more, it could be implantation.
- If the bleeding ramps up to a steady red flow that persists over days, it’s more likely your period.
Tip: Cycles vary. If your cycle is longer/shorter, shift this window accordingly. If you track ovulation (basal body temperature, ovulation predictor kits, or cervical mucus), use ovulation day + 6 to 14 as the likely implantation window.
How to tell the difference (a practical 3-step check)
1) Map the dates
- Note your ovulation window (if you track it) and your expected period date.
- Spotting that appears ~10–14 days after ovulation—especially if it’s very light and brief—fits the typical timing for implantation.
2) Assess the pattern
- Implantation: light, often pink/brown, not soaking period products, may show only when you wipe, typically short (hours to 1–2 days), no clots.
- Period: heavier red flow that usually builds, may include small clots, lasts 2–7 days.
3) Test smartly
- For the most reliable home result, do a urine pregnancy test on or after the first day of your missed period.
- Testing earlier can yield a false negative because hCG may not be concentrated enough in urine.
- If negative but your period still doesn’t start, repeat after 48–72 hours. First-morning urine is more concentrated and can improve early accuracy.
Why symptoms overlap (and confuse us)
The luteal phase hormones (mainly progesterone) can produce breast fullness, mild cramps, mood changes, bloating, and fatigue—symptoms that look like both PMS and very early pregnancy. Some pregnant people never notice implantation bleeding; many non-pregnant people have pre-period spotting due to hormonal fluctuations or cervical irritation. That’s why timed testing and, when unsure, a quick chat with your clinician can help.
When it’s unlikely to be implantation
If you notice any of the following, the bleeding is more suggestive of a period or another cause:
- Red bleeding that soaks pads/tampons/menstrual cups
- Clots or tissue
- Moderate to severe cramps
- Bleeding that lasts >2 days and follows your usual period pattern
Sudden changes in your usual pattern—heavier flow, longer duration, or new severe pain—warrant medical review to rule out conditions like fibroids, polyps, hormonal shifts, or early pregnancy complications.
Red-flag symptoms: seek urgent care now
Bleeding plus any of the following can signal ectopic pregnancy or significant blood loss:
- Severe, sudden, or one-sided lower abdominal pain
- Shoulder-tip pain (referred pain from internal bleeding)
- Dizziness, fainting, looking very pale
- Heavy bleeding (rapidly soaking products) or large clots with severe pain
These are emergencies—do not wait to be assessed.
Testing options and next steps
Home urine tests
- Detect the pregnancy hormone hCG.
- Most accurate on/after the first day of your missed period.
- A faint positive is still positive—repeat in 48–72 hours to see if it darkens, or speak to your clinician.
Blood tests (quantitative hCG)
- It can detect pregnancy earlier and help track whether levels are rising appropriately.
- Your clinician might use serial blood tests and, if needed, an ultrasound to confirm a healthy intrauterine pregnancy or evaluate concerns.
If you’re on fertility treatment (IUI/IVF)
- Progesterone support and procedures themselves can cause light spotting.
- The most reliable answer is your scheduled beta-hCG blood test from the clinic. Early home tests can be misleading, especially if you’ve taken medications that contain hCG.
- Always inform your fertility team about any bleeding or cramping during the two-week wait.
Common scenarios with clear next steps
“I spotted for a day, then nothing.”
This brief pink/brown spotting just before a missed period could be implantation. Test after your period is due; if negative, retest in 48–72 hours. If pain or heavier bleeding develops, seek care.
“I spotted, then the flow ramped up like my usual period.”
That pattern favours a true period. If your flow is heavier than usual (soaking in 1–2 hours, bleeding >7–8 days, or large clots), book a gynaecology consult to check for underlying causes.
“Light spotting with one-sided pain.”
This combination needs urgent assessment to exclude ectopic pregnancy—especially if the pain is severe or you feel faint.
Evidence-based ways to reduce the guesswork
- Track your cycle
Use a calendar or app to log periods, ovulation signs, and any spotting. Over a few months, patterns emerge and help you interpret mid-luteal spotting. If you live with PCOS or irregular cycles, cycle tracking plus clinician input can be especially helpful (see our overview of PCOS and fertility at IVFix: PCOS and fertility). - Time the test
Plan to test on/after the first missed period day. If you test early and it’s negative, it may simply be too soon. Retest after 48–72 hours if bleeding hasn’t started. - Note flow characteristics
Implantation is spotting, not a flow that saturates products. Pink/brown streaks while wiping are more typical; red flow with clots is more period-like. - Listen to your body’s alarms
Severe or one-sided pain, shoulder-tip pain, dizziness, or fainting is not typical of implantation—seek urgent care. - Follow up if patterns change
Sudden changes in bleeding (heavier, prolonged, very painful) deserve evaluation. Depending on your history, your clinician may discuss options ranging from observation and iron studies to imaging and specific treatments. For a broader context about how reproductive health factors affect conception, you may find our piece on IVF success rates useful (what affects IVF success).
Special considerations in the Indian context
- Anaemia is common in people with heavy menstrual bleeding. If you feel unusually tired, breathless on exertion, or look pale, ask about a haemoglobin check.
- Access to early ultrasound may vary. If you have risk factors for ectopic pregnancy (e.g., prior ectopic, tubal surgery, certain infections), mention them early to your clinician to guide timely assessment.
- Nutrition matters: Balanced iron intake (from foods like leafy greens, lentils, jaggery, meats, fortified cereals) and adequate protein support overall reproductive health. Explore our guidance on antenatal nutrition if you confirm pregnancy (antenatal nutrition essentials).
Quick self-checklist (print-friendly)
- Did the spotting occur ~6–14 days after ovulation?
- Is it light, pink/brown, and short-lived (≤2 days) with no clots?
- Are cramps mild or absent?
- Is a pregnancy test due or overdue (on/after the day of the missed period)?
- Any red flags (severe one-sided pain, dizziness/fainting, heavy bleeding, shoulder-tip pain)? If yes, seek urgent care.
Summary you can trust
- Timing: Implantation spotting typically appears right before/around the expected period; a period starts its usual multi-day flow at the expected time.
- Volume & pattern: Implantation is light and brief (no clots; often pink/brown). A period is heavier, red, and sustained with a build-and-taper pattern.
- Testing: The most reliable confirmation is a home urine test after a missed period, repeating after 48–72 hours if uncertain.
- Safety: Severe pain, heavy bleeding, dizziness, or shoulder-tip pain are emergencies—get help immediately.
Conclusion
Light, brief spotting before or around your expected period might be implantation—but the surest way to know is timed testing and, when there’s any concern, a quick check-in with your clinician. Tune into the pattern: colour, volume, duration, and cramps offer strong clues. If you confirm pregnancy, shift focus to healthy early-pregnancy habits; if it’s your period, tracking trends can still reveal valuable insights for your fertility journey.